Hi guys! Sorry I've been MIA for a little. A lot of things going on. Just wanted to check in and post about some of the things I've been using lately that have been helping. The past or month or two have not been the greatest (pain-wise) but I'm convinced things will start to get a little better soon. Myofascial Pain Syndrome is a high maintenance syndrome--I need to do a lot to keep up and feel as normal as possible. Dealing with myofascial pain, to me, is essentially figuring out all my perpetuating factors and figuring out how to correct them (i.e., posture, headaches, balance issues, etc.)
1.
Sleep (at
least 8 hours, or I know I'll feel like shit. Sorry morning people, I won't be around.)
2.
Supplements- I am currently taking B-12 and D for those vitamin deficiencies as well as turmeric, Biotin, Align (probiotic), a multivitamin and a few other random ones. I've really tweaked it down and this is what's working for me. Although the grass is always greener, so I'm constantly looking for new and better things.
3.
Exercise and Wellness- This is been a long process for me. The last few months I was really starting to think I was plateauing. I was discharged from PT but it was hard to get to the gym to do my exercises. Swimming feels great but immediately getting out of the pool, freezes my muscles and puts me back where I started. I also feel it's very important to have a professional watching you to make sure you don't re-injure yourself, which is very easy to do.
LUCKILY, I have a found a trainer I just started with last week who specifically deals with people with chronic pain. I think it's going to go great but it'll take some time to tell. Ultimately, I need to get myself back into shape and straighten all my muscles that have atrophied and this guy will most likely be the best way to make that happen.
Once or twice a month, I am also going to a chiropractor to get realigned and a massage therapist who works at calming down my nervous system. (Fun fact: when you become a chronic pain sufferer, you become conditioned to associate touch negatively from constant poking and prodding.) Massages are slowly starting to feel good and become less painful.
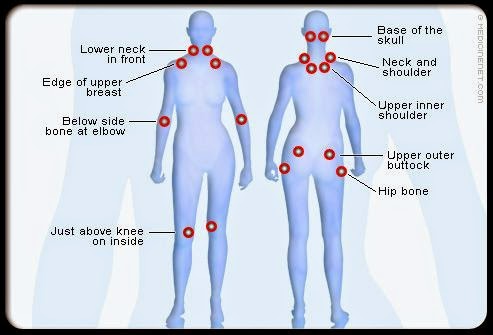
I am also continuing to get injections once or twice a month depending on the severity of the trigger points. My last visit had 8 people total in the room watching me. I am really developing a posse. And I also made them take a picture because I knew no one would believe me. I spent the next hour or so answering questions and lecturing a bunch of 2nd years about MPS and hypermobility. I kind of love explaining medical related things to med students as the girl in fashion. Suck it, med school.
I'm also talking to my therapist when I need her. I think I've been able to handle my stress more lately.
4.
Knowing Your Limits- This seems like it should be pretty simple but is still hard for me to this god damn day. Take breaks before you get pain--whether you're cooking, shopping, whatever. Bring snacks if you get hypoglycemic. Don't be an idiot.
5.
Potential Breast Reduction Surgery- Met with a doctor a few weeks ago after both my doctors suggested breast reduction surgery. My posture is bad and I have a lot of trigger points around my bra areas. I don't think it wouldn't..not help at this point, although it will be miserable to do without pain meds. Sad face. But assuming it will be covered by insurance, I am very excited at the thought of having normal sized boobs.
6.
New and Old Products I am continuing to use for pain-
(Where to buy old products in previous posts. I will link new products.)
China Gel
Kinesio Tape- Like I said earlier, posture is a super important perpetuating factor in dealing with trigger points. Until I can get my breast reduction surgery (and after), I will need to strengthen my muscles to better my posture. You can wear this stuff for a few days and it's pretty water proof, so I even wear it in the shower. I've had PTs put it on me before but I actually prefer the way I do it. You can watch Youtube tutorials but I know what I needed.
RAGE Muscle Therapy Curve Cane- This thing kinda looks like some wild sex toy, but it's just a theracane for athletes. I like it because I hate touching my trigger points. A lot of them are in my neck and shoulders and this crazy thing actually helps sometimes.
Instant Cooling Towel- So guess what store indadvertedly has the best trigger point stuff? Dick's Sporting Goods. Their Sports Recovery section is just ridiculously awesome. You can wet this towel and it'll immediately stay cool for like 2 hours. Cool, right? Good for long car rides, impromptu pain situations. Me likey.
Aches and Pains Shower Gel- This is made with eucalyptus and menthol. Feels good in the shower and lets me do a little more than I usually could post shower. I put it in straight when I get in and let it sit until I'm done to set in.
Emergen-C- This stuff tastes like nasty crap, but I chug it post injections and it seems to help. Has electrolytes, etc. I felt like I recovered much faster than usual.
Ergonomic Computer Stand- Like I said, posture is key. I lay down a lot when I'm on the computer and I'm slowly transitioning over to sitting with this thing and I think it helps.
Amazing Grass Superfood Powder- It's hard to eat healthy when you feel like shit. This green smoothie supplement actually tastes pretty good. I mix it in my nutribullet with some OJ, water and 3/4 of a banana and try to drink one every day.
 |
| Paleo blueberry muffin and green smoothie. Who am I? |
TENS Unit
Nike Roshe Runs- I have flat feet and these are supremely comfy.
Resistance Bands and Stretch Out Hamstring Strap
I'm gonna have a whole closet of shit soon. It's nap time, bai.